Operating and Supervising leads to Planning and Design
In this recent post, I borrowed ideas from industrial engineer Gerry Nadler, who characterized a range of problem types. Two of the problem types that occur all the time in organizations are “operating and supervising” problems and “planning and design” problems.
As Nadler said, operating and supervising “concerns systems and solutions that people participate in routinely, expecting fairly standardized results.”
Every organization produces products or services and so faces operating and supervising problems. Discrepancies between actual results and the expected, standardized results generate both frustrations and opportunities for the people who operate and supervise production.
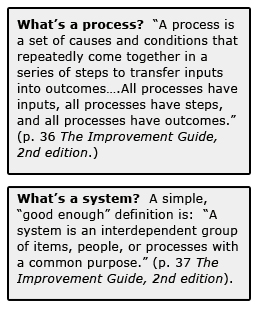
And as people have realized through experience, routine work occurs in a sequence of steps that people can organize and tweak to increase efficiency. In other words, repeated provision of products and services gets done in one or more processes. In turn, you can study and improve these processes.
In contrast to operating and supervising, Nadler said that planning and design involves “custom-made solutions, policies, and designs that restructure existing systems or create new ones.”
The Link Emerges when You Try to Improve Performance of Operations
While not every planning and design situation requires building a production process that you will operate and supervise over repeated cycles, every operating and supervising situation generates planning and design problems.
When you study your production process, you can find opportunities to improve performance—better quality for customers, at lower costs. That’s Deming’s Chain Reaction—see this post.
Good adaptive solutions to operating and supervising problems lead to a restructuring of one or more components of a work process—something has to change. At the point of making a change to a process to improve operations, you are faced with a planning and design micro-problem. As I argued earlier, the Model for Improvement provides the fundamentals to make changes, tweak them, and build them into regular practice.
Example of Planning and Design Problem Embedded in Operating and Supervising Setting
A specialty orthopedic hospital serves about 50 patients a week; each patient gets a new knee or hip joint. The hospital production process has four major steps, with only minor differences between in process steps to treat a patient for hip or knee replacement: preparing the patient for surgery, the surgery itself, immediate recovery and then 24 to 48 hours further recovery and mobility practice before discharge from the hospital. Thus the production process cycles 50 times each week, once for each patient.
Clinicians and managers recognize that most of their patients can return home safely after only two nights in the hospital, if the patients have the right education, home health support and acute care treatment. Some hip replacement patients may be able to go home after only one night’s stay. Last year, data on length of stay showed that most of the knee-replacement patients were staying three nights, while most of the hip replacement patients were staying two nights.
Following process mapping and direct observation of patient care, managers and staff surfaced a bottleneck in mobility treatment: physical therapists were not able to consistently get to each patient within hours of surgery. Getting the patients up and out of bed within hours of the surgery helps patients get home and continue to recover safely, so the lack of consistent PT matched the longer than expected lengths of stay.
Building off programs at other hospitals and their own insights, managers and staff devised a change: deploy people on the unit who can help patients get up and out of bed. The change idea required restructuring the production process on day of surgery nursing care—a planning and design task.
The new “mobility technicians”, drawn from the ranks of certified nursing assistants, were trained by physical therapists from the hospital. Importantly, the MTs are now part of the dedicated orthopedic nursing units and so have greater availability to help mobilize patients on the day of surgery. And since the MTs are also CNAs, dual-trained staff provide the unit supervisors with more flexibility in adjusting to variation in the patient census.
While length of stays have shrunk for patients with no negative effect on safety and recovery, the managers and staff are still revising the way physical therapists work with patients, complementing the work of the mobility technicians. Again, the Model for Improvement’s three questions and test cycle framework should guide effective and efficient redesign.
Maintain the Change and Generate More Improvements: More P&D Opportunities
Of course, once the mobility technicians are working consistently with patients and the physical therapists have adjusted to their new role, the changes need to be defined and maintained as regular practice. Maintaining the change becomes part of the operating and supervising work.
Building a change into the work flow—“implementation”—is the foundation for maintenance.
As colleague and API member Cliff Norman reminded me, Chapter 8 of The Improvement Guide (2nd edition) summarizes many practical points on implementation; check out the implementation checklist on page 185.