Capacity to Add Value
Three weeks ago, I had a discussion with accomplished managers who want to extend their existing dashboard to include financial measures. How should they proceed?
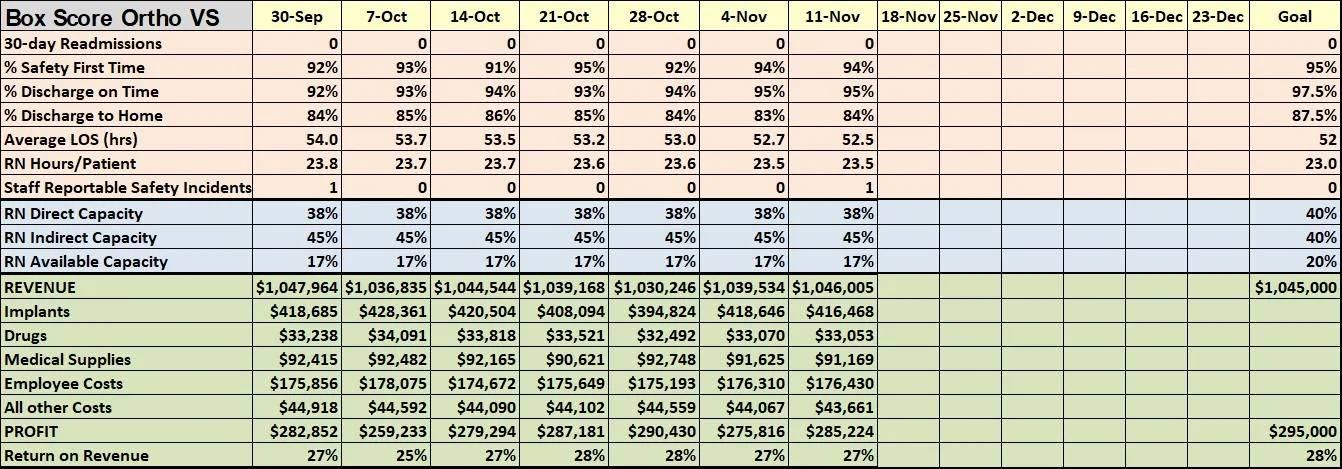
We looked at the Box Score, a key component of Lean Accounting, introduced in two posts here and here.
To recap, the Box Score as described by Brian Maskell aims to provide regular information to people operating a core production process. They use this information to enable them to continuously improve value.
As the picture shows, the Box Score comprises three sets of measures: process performance measures, capacity measures, and financial measures.
Just as in a sports Box Score, the Box Score aims to summarize performance ‘at a glance’. You should choose the Box Score measures so that anyone in the value stream team can understand the numbers. No arcane accounting calculations allowed!
Of course, the power of information only comes when people use the information to act. So as Brian recommends, the value stream managers must regularly look for opportunities to apply Plan-Do-Study-Act to improve performance. They also monitor Box Score measures for unusual spikes or patterns that call for special response.
Capacity Numbers and Improvement
The Box Score includes numbers on direct care and indirect care for key people assigned to work in the value stream.
The Box Score picture shows the capacity for nurses employed by the value stream. ‘Direct capacity’ means hands-on care with the patient, which is our interpretation of ‘value-adding’ activity. Get the number of hours in the week in direct care and divide by the total number of contracted work hours, as a per cent. Indirect capacity includes tasks like documentation, set-up or preparation to provide care, training time and meetings. It also includes work aspects easily seen as ‘waste’ like waiting time and reworking tasks that were not done right the first time. You calculate available capacity by subtraction of direct and indirect capacity from 100%.
Looking at capacity numbers in our example Box Score immediately provoked the lead manager in my meeting to think out loud. How could they decrease indirect capacity and increase direct capacity for key resources? What would those changes mean in terms of revenues and expenses and their existing quality measures?
That’s the power of the Box Score, it stimulates value-stream managers to think and act holistically, reducing the risk of unintended consequences that come from focusing only on quality metrics or only on financial metrics. The capacity measures remind Box Score users to think about the most important work people should do.
More on the vital role of capacity
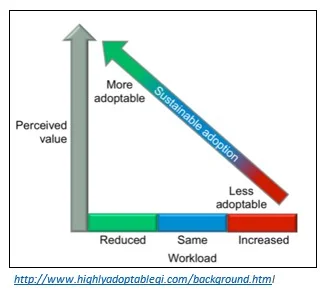
In 2014, Chris Hayes observed two key factors that drive sustainability of changes in health care: (1) the value of the intervention as perceived by an individual or care team who are supposed to apply the changes day to day and (2) the impact of the intervention on the individual or team’s workload.
Valued interventions that reduce workload are the sweet spot for sustainability.
What if changes will increase work?
Chris sketched the picture above to summarize his point—changes that increase work, even if perceived as valuable are simply less likely to be adopted and sustained.
One of my projects right now has summarized changes that will improve health care of older adults. Our faculty experts and testing teams see the changes as valid and valuable.
On the other hand, initial tests suggest the direct care workload will increase even if patients will get better care and avoid complications.
For example, reliable and regular screening for delirium for hospitalized patients means another few minutes of someone’s time every day to prevent problems. Non-pharmacological interventions to prevent or relieve delirium, like orienting a patient to time and place and helping the patient move around out of bed also require somebody’s time.
How are we going to make these age-friendly changes sustainable given the Hayes’ analysis?
The Box Score capacity numbers suggest a solution and challenge for leaders who are interested in their systems becoming age-friendly: before you ask care teams to take on the age-friendly changes, how will you help people in your organization reduce 15 or 20 minutes a day in indirect care? If you can do that, then it is much more likely that care units will be able to sustain our proposed age-friendly changes.